Our research question specifically asked, is education an effective method to combat HIV/AIDS in the U.S. and Africa? Continue reading The Effects of Education on HIV/AIDS Transmission in the US and Africa
Dengue Fever: How Did the U.S. Military Deal with it During the Vietnam War?
https://www.youtube.com/watch?v=-mN3P1Y8t8M
In our presentation we wanted to show the affects and treatments for dengue fever that were done on the US military during the Vietnam War. At the beginning of our video, we wanted to show the US military involvement during the Vietnam War and major dates surrounding this war. The video clip in the middle of our presentation shows how Vietnam was a prime place to spread dengue fever with all of the stagnant water and hot, humid weather. The second half of our presentation mostly focuses on dengue fever; where it comes from and how it spreads. We make note of how the symptoms of dengue fever are similar to the symptoms of a regular fever. The biggest difference is that dengue fever can lead to dengue hemorrhagic fever, which can kill the patient in 24-72 hours. The biggest form of treatment for dengue was preventative. With that, the popularity of DDT and other pesticides rose were used to kill mosquito breeding grounds. Other measures the military used was instructing their ground forces to wear long sleeve shirts and pants to show less skin and make it harder for the existing mosquitos to spread the disease. Actual treatment for dengue fever was the same as a normal fever; fluid replacement and rest. The lack of medical laboratories the military had during the war made it extremely difficult for physicians to diagnose fever patients with dengue fever. Although the United States’ Military did not have a specified way of treating Dengue Fever, they had a way of attempting to prevent it. Once military personnel contracted the disease the United States’ military took all the measures necessary to help the soldier’s and keep them from getting Dengue Hemorrhagic Fever or Dengue Shock Syndrome. The point of this video was to shed light on how the United States’ Military is able to prevent a potentially deadly disease, as well as adapt to treatment once it was contracted
Karlie Hightower
Alex Page
Methods of Treatment for Yellow Fever
Yellow Fever has been one of the most dreaded diseases since the early 1700s. It wasn’t until 1901 that mosquitoes were proven to be the transmitters of the disease. Aedes aegypt is the species that carries it Several scientists entertained the idea, beginning with Josiah Nott in 1850 followed by Carlos Finlay in 1881. Sadly, these scientist were made a mockery of because of the incompetence of their peers. Timeline of the history of Yellow Fever treatment.
What is Yellow Fever?
Yellow fever is an acute systemic illness
Jungle yellow fever –this form of yellow fever originates in warm ,wet climates. It is spread by jungle mosquitoes and mainly affects monkeys. If a human were to visit the jungle and be bitten by an insect who bit an infected monkey, they too can contract the disease..
Urban yellow fever – this is spread when an Aedes aegypti mosquito bites an infected human or monkey and then goes on to bite other people. Urban yellow fever is most likely to occur in settlements close to the jungle, where infected monkeys and mosquitoes live. Urban yellow fever is extremely rare in the Americas. Put simply, a human may go into the jungle, be bitten by an infected mosquito, come back to their settlement, and infect mosquitoes who bite them there; those mosquitoes will then infect other people.
What are its symptoms?
In severe cases yellow fever causes a high fever, bleeding into the skin and the death of cells in the liver and kidneys. Liver damage results in severe jaundice – yellowing of the skin; hence the name “yellow fever”.

Prof. Frank Hadley Collins, Dir., Cntr. for Global Health and Infectious Diseases, Univ. of Notre Dame
This 2006 photograph depicted a female Aedes aegypti mosquito while she was in the process of acquiring a blood meal from her human host, who in this instance, was actually the biomedical photographer, James Gathany, here at the Centers for Disease Control. Youll note the feeding apparatus consisting of a sharp, orange-colored fascicle, which while not feeding, is covered in a soft, pliant sheath called the “labellum, which retracts as the sharp stylets contained within pierce the host’s skin surface, as the insect obtains its blood meal. The orange color of the fascicle is due to the red color of the blood as it migrates up the thin, sharp translucent tube.
Where did it come from?
Experts believe yellow fever originated in Africa and was introduced to South America via the slave trade in the 16th century. Several major yellow fever epidemics have taken place in Europe, the Americas and Africa since the 17th century. It was deemed one of the most dangerous infectious diseases in the 19th century.
Methods of Treatment
In the 1850s, people used isolation as their method of treatment. They had no idea of how to treat an illness that they knew nothing about. Many cities would stop trade and visitation with others if rumors were heard of infection within the area. This method of treatment was helpful for some areas, but others not so much. In 1901, Walter Reed, made a connection between the mosquitoes being transmitting agents of yellow fever and actually provided proof so that it was believable. Shortly after knowledge was gained, the U.S army began fumigating breeding grounds for the mosquitoes to decrease the amount disease cases.
http://www.medicalnewstoday.com/articles/174372.php
http://www.historyofvaccines.org/content/timelines/yellow-fever
https://historyofcollierville.wikispaces.com/Yellow+Fever
http://en.wikipedia.org/wiki/Yellow_fever
Eradication of Malaria in the United States
The fight between humans and Malaria has been long and wide spread. Its a struggle in which we have often found ourselves bested. Our research question deals with this fight, specifically how it played out in America. Although the name Malaria may not have been used, the sickness has been documented by many of the great world civilizations throughout history.
The earliest known reference to the symptoms of Malaria is found in an ancient Chinese document, known as the Cannon of Medicine, or the Nei Ching; this document dates to 2700 BC. Other early references come from forth century Greece, where Malaria caused a serious decline of many of the city states. The sixth century Sanskrit medical treatise, Susruta, linked the sickness to insect bites and many Roman writers made a connection between Malaria and swamps.
Continue reading Eradication of Malaria in the United States
Chlamydia: Why the South?-A Look at Possible Contributing Factors
Project By: Rae Mann, Caroline Roberts, and Meredith Moore
Back in February, Dr. Peterson brought to our attention the daunting numbers of sexually transmitted diseases contracted within our population. Continue reading Chlamydia: Why the South?-A Look at Possible Contributing Factors
Oh No, It’s Polio!
What encouraged eradication efforts in the 1940s and 1950s that would lead to the widespread use of the Polio vaccine?
An examination by Kendall Carney and Kristin Conwill
The Basics
What is Polio, anyway?
According to the World Heath Organization,
“Polio is a highly infectious disease caused by a virus. It invades the nervous system, and can cause total paralysis in a matter of hours. The virus is transmitted by person-to-person spread mainly through the fecal-oral route or, less frequently, by a common vehicle (e.g. contaminated water or food) and multiplies in the intestine. Initial symptoms are fever, fatigue, headache, vomiting, stiffness in the neck and pain in the limbs. One in 200 infections leads to irreversible paralysis (usually in the legs). Among those paralyzed, 5% to 10% die when their breathing muscles become immobilized.”
Furthermore,
“Polio mainly affects children under 5 years of age,” (who.int).
Background
Check out our timeline!
http://timeglider.com/t/b90db8b9f47006d7?min_zoom=1&max_zoom=100s
Gaining Support
The March of Dimes
- In 1934, Basil O’ Connor, Roosevelt’s adviser, hosts a ball in honor of Roosevelt’s birthday and to raise money for polio research.
- After 4 years of success, Roosevelt creates his own foundation named National Foundation for Infantile Paralysis.
- Later in 1938, Eddie Cantor broadcasts the idea of people mailing dimes to the White House in support of Roosevelt’s new foundation on his radio show.
- Grass root organizations and celebrity sponsors joined the campaign coining the name, March of Dimes.
- March of Dimes became instantly popular and continued to grow. With FDR busy running the country, he delegated the role of President of March of Dimes to Basil O’Connor.
- O’Connor was President for 30 years.
- His first goal was to create local chapters throughout the nation to raise funds and provide aid in order to quickly respond to outbreaks in the region.
- Proved to be a highly effective use of funds and entering 1950 there was 3,100 different chapters run mostly through volunteers.
- Little was known about polio and barely any government money went to public health, research and health care was nonexistent.
- 1951: $1 million had been put towards research to identify all types of polio.
- 1955: $9 million went towards the testing and production of Salk’s vaccine to guarantee the safety and effectiveness of the product before distributing.
- Demonstrates how fearful people were that they would gamble away $9 million in order to ensure its safety before distribution.
- March of Dimes gives research grant to John Enders, Thomas Wellers, and Frederick Robbins who discovered how to grow polio virus in non-nervous tissue.
- O’Connor and Salk became fast friends after meeting in Second International Poliomyelitis Conference in Copenhagen.
- This friendship led to a lot of beneficial polio research and development projects using March of Dimes funding.
- In 1960, March of Dimes builds Salk an institute for biological studies in San Diego
- Being founded by Roosevelt, the foundation had a lot of support immediately. His National Foundation’s balls garnered support from the upper class immediately.
- March of Dimes campaign enacted by Eddie Cantor drew in the middle and lower class by presenting the idea that every dime makes a difference.
- Fundraising appeals made by Elvis, Lucille Ball, Mickey Rooney, Zsa Gabor, Helen Hayes, etc…
The Aspect of Fear
In addition to public campaigns, the element of fear was a powerful influence on new and quick approaches for a Polio vaccine. The US suffered a rising number of cases each summer that lowered morale, especially following WWII. The public reaction and “solutions” to outbreaks also caused concern and distress within communities. Fear of Polio contributed to the rapid efforts of working towards a cure through the amount of outbreaks and reactions to them.
Polio started to become more noticeable with the 1916 outbreak in New York. The cases that summer reached 26,212 and continued to grow in different parts of the country in the following decades. The chart below demonstrates the growing number of cases until the 1952 epidemic effecting thousands (Pomerantz, 3).
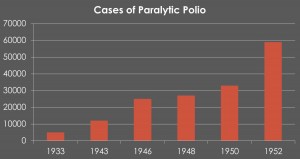 Though outbreaks tended to effect one area or another at a time, most of the nation as a whole saw devastating numbers throughout the years. The map below illustrates the number of Polio notifications before the vaccination. These cases are totaled from 1910-1955 (Trevelyan, Smallman-Raynor, and Cliff, 276).
Though outbreaks tended to effect one area or another at a time, most of the nation as a whole saw devastating numbers throughout the years. The map below illustrates the number of Polio notifications before the vaccination. These cases are totaled from 1910-1955 (Trevelyan, Smallman-Raynor, and Cliff, 276). Due to the large spread of the disease, efforts were enforced within cities in an attempt to control Polio. These efforts, however, contributed to the anxiety felt about Polio without much success in defeating the disease or preventing the spread. Among the efforts were quarantining and closing public facilities like schools, pools, and churches. The shutdown of public meeting spaces was also aided by sanitation efforts around cities and towns. Attempts such as these only contributed to and demonstrated the widespread fear of Polio (Wellner, 55).
Due to the large spread of the disease, efforts were enforced within cities in an attempt to control Polio. These efforts, however, contributed to the anxiety felt about Polio without much success in defeating the disease or preventing the spread. Among the efforts were quarantining and closing public facilities like schools, pools, and churches. The shutdown of public meeting spaces was also aided by sanitation efforts around cities and towns. Attempts such as these only contributed to and demonstrated the widespread fear of Polio (Wellner, 55).
The disease had a history of taking the nation’s children’s lives, which, following WWII was a psychological hit to American families. Franklin Roosevelt appealed to a radio broadcast for donations by stating,
“The dread disease that we battle at home, like the enemy we oppose abroad, shows no concern, no pity for the young. It strikes—with its most frequent and devastating force— against children. And that is why much of the future strength of America depends upon the success that we achieve in combating this disease,” (Historyofvaccines.org).
The effect Polio had on children was psychologically devastating to the nation. Mark Sauer, a Polio survivor, notes that,
“polio left kids crippled, and that was an image that this big strong postwar country simply couldn’t abide. We had children lining up in wheelchairs, in iron lungs, whose very vitality [was drained] and everyone’s hope for their future…[shaken] right at the most critical time in their childhoods,” (Wellner, 54).
Polio was a disease that took America’s youth in a time when the country was recovering from a long lasting war. The nation needed to work together to defeat this source of anxiety and depression introduced into its society year after year.
Results!
Efforts due to the March of Dimes Campaign and fear led to the discovery of vaccinations at last. There are four notable dates and developments. The first was in 1935 with the discovery of three vaccines. Unfortunately, they had disastrous results. The second was in 1948 with the test trials by Hillary Koprowski and Tom Norton. Not yet aware that there were three types of polio, this vaccine only developed antibodies for Type II. 1952 was a monumental year with Jonas Salk’s work on the vaccine that could kill all three types of Polio. The vaccine he created was finally approved and licensed in 1954. Finally, in 1959 Sabin created an attenuated vaccine for the Soviet Union. It was taken orally, cheaper, and worked faster, therefore the U.S. adopted it from 1963 – 1999. Vaccines were discovered so the fight was essentially won (marchofdimes.org).
So, what’s the verdict?
The March of Dimes campaign and fear due to reoccurring Polio outbreaks encouraged eradication efforts in the 1940s and 1950s that would lead to the widespread use of the Polio vaccine.
Sources, Sources, Sources
“History of Polio.” Global Polio Eradication Initiative Polio and Prevention. The Global Polio Eradication Initiative, 2010. Web. 18 Apr. 2015. <http://www.polioeradication.org/Polioandprevention/Historyofpolio.aspx>.
“History of Polio.” History of Vaccines RSS. The College of Physicians of Philadelphia, 2015. Web. 18 Apr. 2015. <http://www.historyofvaccines.org/content/timelines/polio>.
“History.” PolioToday. Web. 11 April 2015. http://poliotoday.org/?page_id=13
“NMAH | Polio: Timeline.” NMAH | Polio: Timeline. Smithsonian, 2015. Web. 18 Apr. 2015. <http://amhistory.si.edu/polio/timeline/>.
“Poliomyelitis.” World Health Organization. Web. 11 April 2015. http://www.who.int/mediacentre/factsheets/fs114/en/
Pomerantz, Lauren. “Living in Fear: America in the Polio Years.” Teachspace.org. Web. 11 April 2015. http://www.teachspace.org/personal/research/poliostory/fear3.html
Rose, David. “History.” A History of the March of Dimes. March of Dimes, 26 Aug. 2010. Web. 18 Apr. 2015. <http://www.marchofdimes.org/mission/a-history-of-the-march-of-dimes.aspx>
“Salk Institute – About Salk – History of Salk – Discovery Timeline.” Salk Institute – About Salk – History of Salk – Discovery Timeline. Salk Institute For Biological Studies, 2015. Web. 18 Apr. 2015. <http://www.salk.edu/about/discovery_timeline.html>.
Sass, Edmund. “Polio History Timeline.” Polio History Timeline. University Press of America, 11 Jan. 2005. Web. 18 Apr. 2015. <http://www.eds-resources.com/poliotimeline.htm>.
Trevelyan, Barry, Matthew Smallman-Raynor, Andrew Cliff. “The Spatial Dynamics of Poliomyelitis in the United States: From Epidemic Emergence to Vaccine-Induced Retreat.” Annals of the Association of American Geographers, 95.2 June (2005): 269-293. JSTOR. Web. 11 April 2015. http://www.jstor.org/stable/3694119
Wellner, Karen L. “Polio and Historical Inquiry.” OAH Magazine of History, 19.5 September (2005): 54-58. JSTOR. Web. 11 April 2015. http://www.jstor.org/stable/25161982.
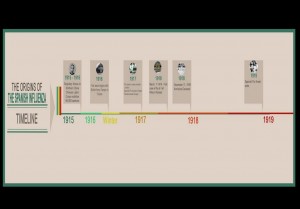
Spanish Flu
HIV/AIDS Epidemic in the United States from 1980-2000

One of the largest misunderstandings concerning HIV/AIDS is the difference between the two diagnoses. HIV is the predecessor to an AIDS diagnosis, although they are the same virus.
What is HIV?
HIV, or Human Immunodeficiency Syndrome, is a virus that attacks the immune system. Unlike with most virus, the human body cannot clear the HIV infection. A diagnosis of HIV depends upon the presence of HIV antibodies within a person.
What is AIDS?
AIDS, or Acquired Immunodeficiency Syndrome, is the final stage of an HIV infection. A diagnosis of AIDs requires that an HIV positive individual have one or more opportunistic infections, certain types of cancer (Karposi’s Sarcoma) or a very low CD4 count.
At the beginning of the HIV/AIDS epidemic the biggest question was “Where does HIV/AIDS come from?”
Rumors of where HIV/AIDS originated from were extremely popular throughout the 1980s when the epidemic seemed to be spreading uncontrollably. Two of the largest rumors were that HIV/AIDS was transmitted through the polio vaccine or that HIV/AIDS came from a “Patient Zero” who originally contracted the virus and then it cascaded to all infected people.
Continue reading HIV/AIDS Epidemic in the United States from 1980-2000
Post Polio
The Fate of Poliomyelitis after Salk’s US Campaign
Brooke Bandon, Marie Videau and Mattie DeCella
History of Polio after Salk
1957: Start of the first oral poliovirus vaccination tests in the Democratic Republic of Congo
1961: Dr. Albert Sabin develops an oral vaccination, it rapidly becomes the vaccine of choice against polio.
1968: Salk’s vaccine was no longer routinely used in the US, until reappearance in 1997.
1970’s: Surveys show that polio is widespread in many developing countries, which leads to the routine immunization of polio.
1985: Rotary International launches PolioPlus.
1988: Global Polio Eradication Initiative is launched; vows to eradicate polio by year 2000.
1994: polio declared eliminated in the Americas.
1996: Nelson Mandela launches “Kick Polio Out of Africa campaign” leading to 420 million children in Africa being vaccinated.
2001: 35 million children in Afghanistan and Pakistan vaccinated.
2002: Polio eradicated from Europe.
2003: In Northern Nigeria, campaigns are suspended because of rumors about the safety of the vaccine. A new outbreak occurs.
2006: Four endemic countries remain: Afghanistan, India, Nigeria, and Pakistan. Outbreaks ended in Yemen and Indonesia.
2009: New bivalent oral poliovirus vaccine used in Afghanistan.
2011: People stop getting vaccinations because of the CIA going in and claiming to be giving vaccinations when they were not.
2014: South-East Asia region declared polio free.
Polio Eradication and Endgame Strategic Plan 2013-2018
A plan was developed by the Global Polio Eradication Initiative (GPEI) with the help of national health authorities, scientific experts, donors, and other global health initiative in response to the World Health Assembly. The polio eradication and endgame plan addresses the eradication of all polio disease while planning for the backbone of the polio effort to be used for delivering other health services to children. They even set up an Emergency Action Plan to be used.
State the Facts
- Polio cases have decreased by over 99% since 1988, from an estimated 350,000 cases in more than 125 endemic countries then, to 416 reported cases in 2013.
- These included only 160 cases in endemic countries; international spread from endemic areas into polio-free areas accounted for the remainder.
- In 2014, only 3 countries (Afghanistan, Nigeria and Pakistan) remain polio-endemic, down from more than 125 in 1988.
- In 2014, only parts of 3 countries in the world remain endemic for the disease–the smallest geographic area in history. Of the 3 strains of wild poliovirus (type 1, type 2, and type 3), wild poliovirus type 2 was eradicated in 1999 and case numbers of wild poliovirus type 3 are down to the lowest-ever levels with the no cases reported since November 2012 from Nigeria.
WPV v. cVDPV
WPV: wild poliovirus
cVDPV: circulating vaccine-derived poliovirus
- Occurs from a genetic mutation in the strain, rarely, and only in the right circumstances. (On rare occasions, if a population is seriously under-immunized, an excreted vaccine-virus can continue to circulate for an extended period of time. The longer it is allowed to survive, the more genetic changes it undergoes. In very rare instances, the vaccine-virus can genetically change into a form that can paralyse – this is what is known as a circulating vaccine-derived poliovirus (cVDPV). It takes a long time for a cVDPV to occur. Generally, the strain will have been allowed to circulate in an un- or under-immunized population for a period of at least 12 months. Circulating VDPVs occur when routine activities are poorly conducted and a population is left susceptible to poliovirus, whether from vaccine-derived or wild poliovirus. Hence, the problem is not with the vaccine itself, but low vaccination coverage. If a population is fully immunized, they will be protected against both vaccine-derived and wild polioviruses.)

India: 524
Nigeria: 1
Pakistan:215

India: 225
Nigeria: 335
Pakistan: 103

India: 1
Nigeria: 62
Pakistan: 198

India: 0
Nigeria: 0
Pakistan:21
Resources:
https://extranet.who.int/polis/public/CaseCount.aspx
http://www.polioeradication.org/Infectedcountries/Pakistan.aspx#sthash.4llgnOMd.dpuf
http://www.polioeradication.org/Portals/0/Document/InfectedCountries/Pakistan/2014_NEAP_Pakistan.pdf
http://www.polioeradication.org/Portals/0/Document/InfectedCountries/Afghanistan/AnnualReport_PEI_Afgh_2013.pdf
http://www.polioeradication.org/Infectedcountries/Nigeria.aspx
http://www.polioeradication.org/Portals/0/Document/InfectedCountries/Nigeria/Nigeria_NationalPolioEradicationEmergencyPlan_2014.pdf
http://www.who.int/mediacentre/news/releases/2013/polio_six_year_plan_20130425/en/
http://www.who.int/mediacentre/factsheets/fs114/en/
The Yellow Fever Epidemic of 1793 from Haiti to the US
The Spread of Yellow Fever from Haiti to the U.S.
Yellow Fever has had a long history on the island of Haiti. British troops felt its devastating effects as early as 1793. Later in 1802 French troops were sent by napoleon to put down a slave revolution. More than 70% of the initial 30,000 scummed to yellow fever. With Yellow Fever killing most of the French Troops the Anti-Colonial force lead by Toussaint Louverture was able to take back control of Haiti. French Slave owners fled the island for locations such as New Orleans and Philadelphia. Yellow fever traveled with these men to the United States and had a profound effect on cities such as Philadelphia.
So why do we talk about the Yellow Fever epidemic in Philadelphia and not New Orleans? In 1763 the Spanish government of New Orleans banned the immigration of enslaved Haitians to the city. This ban was in response to the Haitian revolution. Southern slave holders did not want their slaves influenced by Haitian revolutionaries. This ban forced Haitian farmers and their slaves to find another place to go. They landed in port cities along the east coast where the ban did not exist, such as Charleston SC, Norfolk VA, and Philadelphia PA. Haitian planters and their slaves brought yellow fever with them to these port cities. Yellow Fever hit these ports hard because people in America had no immunities to this tropical disease. The following timeline tracks down the spread of Yellow Fever from Haiti to the United States:
http://timeglider.com/t/84232ee2a7b74919?min_zoom=1&max_zoom=100
Yellow Fever in Philadelphia
Yellow fever had originally struck Philadelphia around 1747, but the city managed to contain the disease quickly. However, in 1793, yellow fever made its way to Philadelphia once again and this time ravaged the entire city, killing 5,000 people out of a total population of 45,000 between August 1st and November 9th of 1793. In addition to this number, it is estimated that 17,000 people fled from the city (Source: http://www.history.com/this-day-in-history/yellow-fever-breaks-out-in-philadelphia and http://www.eyewitnesstohistory.com/yellowfever.htm).
Benjamin Rush, a local physician, managed to keep a recording of the various patients he treated for yellow fever as well as his thoughts regarding the causes and treatments for the disease. Rush’s notes on the epidemic in Philadelphia indicate that physicians of that time period had discovered that yellow fever was found in two stages and differed in symptoms and degree in patients. However, treatments included purging and bleeding; a sign that the scientific community still believed that the yellow fever was related to the four humors (Source: http://deila.dickinson.edu/theirownwords/title/0020.htm-“About the book”).
The link to the interactive timeline below focuses on these months and depicts some of the cases noted by Rush as well as key dates regarding the spread of Yellow Fever in Philadelphia in 1793:
http://timeglider.com/t/2ead2a3533b7f924?min_zoom=1&max_zoom=100
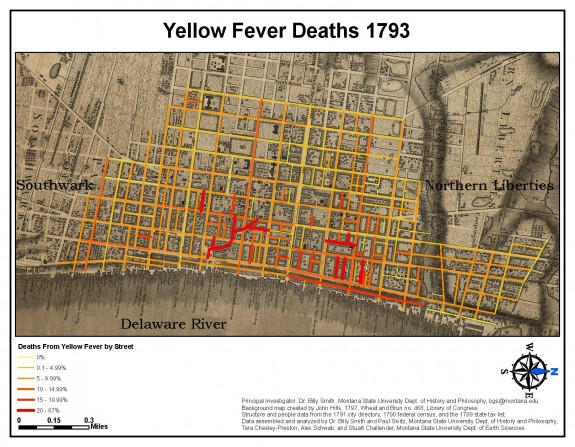
Coastal port cities were most vulnerable to early outbreaks of Yellow Fever. Not only were these areas high traffic ports, but also they were rapidly growing areas with tightly packed populations. Many of the traffic in the ports were from traveling merchants and also refugees from Haiti, contaminated with Yellow Fever when they arrived in port. The first cases of Yellow Fever in the United States started to appear in the 1790s, in the cities of New York, Charleston, Philadelphia, and New Orleans.Throughout the next century, thousands of Americans died and even more became sick with the fever. In many places of the United States, as much as ten percent of the population died every year from epidemics of Yellow Fever.
The southern region of the United States was most affected by Yellow Fever up until the early 20th century. The temperate climate made optimal breeding grounds for the mosquitoes carrying Yellow Fever. The areas of the south were also less organized than Northern cities because of a rapidly growing population of those areas. The port town of New Orleans suffered considerably during the late 18th and early 19th centuries. In 1796 and 1799, major epidemics killed 600 people combined which was between five and ten percent of the population at the time. The invention of the steamboat and extensive railroad networks carried the disease throughout the United States into the interior, especially in the South.
Northern cities suffered their last epidemic in 1822 with the large epidemic in New York City. At this point, quarantines and isolation measures for infected sailors and passengers exhibiting symptoms at port were put into place and seemed to be working well to control the Yellow Fever north of Virginia. Southern cities were slower to adopt quarantine measures and could not keep up with their explosive growth in population in order to control their public heath. This caused the large number of deaths and epidemics in the South with only a brief period of relief during the Civil War. Northern blockades and restriction of trade of Southern ports may have been detrimental to the South’s economy during the war, but was a major reason Yellow Fever epidemics were almost non-existent during this time period.

Want to learn more about the spread of Yellow Fever? Check out these great sources that were used in our research:
- pbs.org/wgbh/amex/fever/map/
- http://wwww.ncbi.nlm.nih.gov/pmc/articles/PMC1750233/?page=2
- http://pabook.libraries.psu.edu/palitmap/YellowFeverHaulingDead.jpg
- http://www.tip.sas.upenn.edu/curriculum/units/2009/02/09.02.09.pdf
- “African American Migration Experience.” AAME :. Accessed April 22, 2015. http://www.inmotionaame.org/migrations/landing.cfm?migration=5&bhcp=1.
- Marr, John S., and John T. Cathey. “The 1802 Saint-Domingue Yellow Fever Epidemic and the Louisiana Purchase.” Journal of Public Health Management and Practice: 77-82.
- http://philadelphiaencyclopedia.org/archive/yellow-fever/yellow-fever-1793-jpg/
- http://faculty.humanities.uci.edu/bjbecker/PlaguesandPeople/week7c.html
- http://deila.dickinson.edu/theirownwords/title/0020.htm
- http://www.eyewitnesstohistory.com/yellowfever.htm
Pictures for the Philadelphia Yellow Fever Timeline found in the following sources:
- http://pabook.libraries.psu.edu/palitmap/YellowFeverHaulingDead.jpg
- http://www.tip.sas.upenn.edu/curriculum/units/2009/02/09.02.09.pdf
- https://en.wikipedia.org/wiki/Andrew_Hamilton_(lawyer)#/media/File:Andrew_Hamilton_Bush_Hill_Drawing.png
- http://29deadpeople.com/wp/?page_id=444
- http://www.historyforkids.org/learn/science/medicine/yellowfever.htm
- https://www.globalcitizen.org/en/content/these-9-historical-quarantines-can-teach-us-a-lot/
This blogpage was created by Adrika Venkatanarayanan, Cody White and Allison Terry